☆☆☆☆☆ 4.5 Star Rating Nitetronic – The Manufacturer of The GoodNite Anti-Snoring Pillow
Nitetronic, the company behind the Goodnite anti snore pillow, claims to be the first and the only clinically proven anti-snoring smart pillow currently on the market. The German-based company was established in 2012 and their product was an instant success in Europe.
Nitetronic is based out of Hamburg, Germany where all of the research and development was performed. Their manufacturing facility is located in Shanghai China. What started out as a small company in 2012 has now spread globally with distribution centers in Canada, Thailand, Japan, Hong Kong, China, Netherlands, and Europe. On August 1st, 2016, the GoodNite pillow was introduced to the United States and Canada when the company opened Nitetronic America LLC in Upland, California.
The first generation GoodNite Pillow was released in 2012 and in January 2016, an improved second generation Goodnite pillow was released which offers improvements in comfort as well as advancements in the algorithm which controls the pillow and an updated version of the app – NiteLink2.
About the GoodNite Smart Pillow
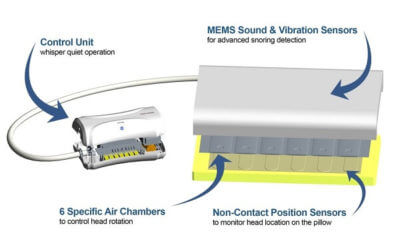
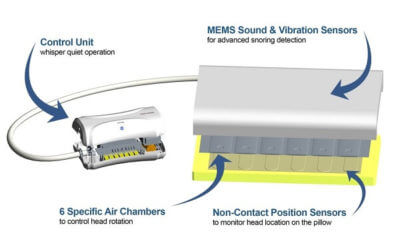
 At first glance, the GoodNite Pillow may seem a bit daunting. The unit contains a pillow with a hose exiting from it which connects to a control box. In addition, there is a smartphone app that is also used.
At first glance, the GoodNite Pillow may seem a bit daunting. The unit contains a pillow with a hose exiting from it which connects to a control box. In addition, there is a smartphone app that is also used.
My first reaction was “Wow, how the heck does this thing stop snoring?” After reading and digesting all the information that I could find online, I was no longer intimidated by this pillow but rather intrigued, as I was then able to see exactly how such a device could actually work. As it turns out, the unit is able to operate independently from the phone app, although the app does offer valuable information as well as provides evidence that the pillow is actually working by recording how much you snore throughout the night along with a plethora of other information. It establishes a baseline by recording snoring habits for three nights prior to activation. This allows you to perform a before and after analysis to determine whether or not the Goodnite pillow is effective.
The Anatomy of The GoodNite – How The GoodNite Works
 The GoodNite is a queen size pillow, measuring 24″ X 14.5″ X 3″. The pillow can be fitted with a standard pillowcase which can be exchanged to keep it clean and fresh.
The GoodNite is a queen size pillow, measuring 24″ X 14.5″ X 3″. The pillow can be fitted with a standard pillowcase which can be exchanged to keep it clean and fresh.
Inside the pillow, there’s a polyester filled pocket on both the top and bottom face of the pillow. In the middle, is the working parts of the pillow which are responsible for monitoring snoring and head position as well as inflating the air chambers.
What makes this pillow unique is the fact that there are six individually controlled air chambers that run horizontally along the full length of the pillow. Each chamber has three bags that are stacked on top of each other. Also within the pillow is a series of MEMS sensors which are able to detect the noise and vibration associated with snoring. With the machine turned on, these sensors are constantly listening for the sound of snoring. When snoring is detected, the sensors deliver the message to the control unit informing it of the snoring and the exact head position. The control unit then responds by activating the built-in air pump which delivers air through the tubing into one or more of the six air chambers. The end result is that the chambers slowly inflate where needed and the head is slowly shifted to the side which opens the airway and stops the snoring. The sensors continue monitoring and making adjustments throughout the night. This design is unique in comparison to other inflatable smart pillows that I have seen which are only capable of raising or lowering the head and contain only a single air chamber which does not necessarily shift the head left or right.
An initial concern that I had with this product was that the constant slow movement of my head would keep me up all night.
Within the Goodnite study (mentioned below), it was stated in the conclusion that there was “no deterioration of the sleep and breathing sleep disturbances” related to the active head position changes. In other words, the head movements are gentle enough not to wake you up. My fears were put to rest knowing that this information was coming from an actual published study which was conducted in a sleep lab using sophisticated equipment that monitors breathing, heart rate, brain wave activity, etc.
Why Does It Work?
 The technology behind the Goodnite pillow is indeed fascinating but this leaves one very important question – How does slowly moving the head to the side while asleep prevent snoring?
The technology behind the Goodnite pillow is indeed fascinating but this leaves one very important question – How does slowly moving the head to the side while asleep prevent snoring?
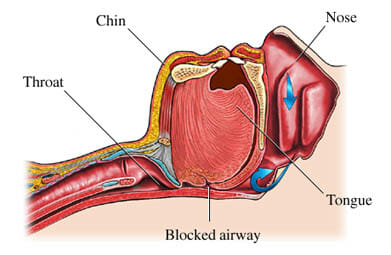
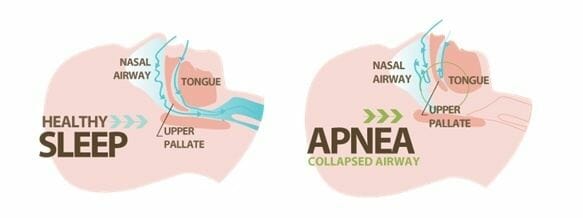
While asleep, the tongue, as well as other muscles within the airway, tend to relax and fall back which often obstructs the airway. This problem is more prevalent in those who are overweight and are older. While breathing through an obstructed airway, oxygen is forced through this narrow obstructed opening and tissue within the airway begins to collide which in turn causes the sound of snoring.
A surprising number of snorers can treat their snoring by simply moving their body or head to one side which permits free breathing. This is possible because moving the head to one side reduces the effects of gravity on the airway. This is referred to as positional therapy and is the reason why a smart pillow may be effective.
Not convinced? Try this: relax, lay back and mimic the sound of snoring. Next, continue to create the snoring sound and slowly shift your head to the left or right. Be sure not to alter the intensity of your “snoring”. When you turned your head, did you notice that the sound of snoring was greatly reduced or even eliminated? If this is the case, this pillow may be a good choice for you.
How Much Does the GoodNite Cost?
 How much do you expect to pay for such a product? It seems as if a lot of effort and capital have been invested in bringing this device to market, so I wouldn’t expect it to be inexpensive. The retail price for the GoodNite pillow is currently set at $299. Nitetronic does offer free shipping which is, of course, nice considering that it’s a fairly large investment.
How much do you expect to pay for such a product? It seems as if a lot of effort and capital have been invested in bringing this device to market, so I wouldn’t expect it to be inexpensive. The retail price for the GoodNite pillow is currently set at $299. Nitetronic does offer free shipping which is, of course, nice considering that it’s a fairly large investment.
In comparison to other product that is similar in nature, the GoodNite is competitively priced.
Risk-Free Trail and Warranty
Nitetronic backs their product with an impressive 30-night risk-free trial in which they allow you to test their pillow for 30 nights prior to deciding whether to keep it or not. The trial period begins the day that you receive it and ends 30 days later. This will give you enough time to acclimate to a new pillow as well as monitor your progress with their smartphone app. According to Nitetronic, after establishing a baseline with the app, you should notice results the first night that it’s activated and every night thereafter. This guarantee seems fairly generous, considering that this is an expensive piece of equipment that can be returned.
There is one caveat which is that returns are subject to a $50 restocking fee.
The GoodNite pillow is backed by a 1-year limited warranty which begins on the date of purchase and covers defects in material and workmanship while under normal use. The warranty can not be transferred and does not cover abuse, misuse or normal wear and tear. Nitetronic covers return shipping for warranty claims.
Can the Nitetronic Pillow Be Used Instead of A CPAP?
If you are currently using a CPAP to treat Obstructive Sleep Apnea, you may be wondering if the Nitetronic pillow can serve as a replacement for your CPAP. This product has been studied for the treatment of snoring only and not OSA. Because of this, you should not replace your CPAP with the GoodNite pillow. According to the manufacturer, you could potentially use this pillow as a supplement for your CPAP, but not as a replacement. As always, you should first speak with your physician prior to making this decision.
Nitetronic Goodnite Pillow vs Smart Nora
 Smart Nora, one of Nitetronic’s only competitors, offers a similar product that’s used to stop snoring. There are however a few key differences between the two.
Smart Nora, one of Nitetronic’s only competitors, offers a similar product that’s used to stop snoring. There are however a few key differences between the two.
The first difference has to do with the location of the sensor(s) which monitor the sound of snoring. The Goodnite pillow has sensors integrated into the pillow which are able to identify snoring as well as locate the position of the head. When the sound of snoring is detected, this information, as well as the position of the head, is transmitted through a wire that is housed within the cord connecting the pillow to the control unit.
In contrast, the Smart Nora uses a “pebble”, which is a small wireless device that is about the size of a computer mouse, to listen for the sound of snoring. It’s placed on the nightstand or mounted directly above the head. When snoring is detected, it sends a wireless signal to the controller which responds as needed. The Nora, however, does not feature head position sensors.
Another key difference between the two has to do with the air bladder which inflates and deflates. With the Nora, a single air chamber inflates and deflates in order to move the head up or down which stimulates the airway just enough to cause it to tighten and prevent snoring.
In contrast, the Goodnite pillow contains six individual air chambers that work together to actually rotate your head from one side to another in order to provide a clear path for air to flow. The pillow sensors detect the sound of snoring as well as head position and use this information to inflate one or six chambers to rotate the head to the left or right.
Finally, the Nora allows you to place their insert inside of your regular pillow while the Goodnite components are integrated into a provided pillow.
These two products do share several similarities. Both smart pillows allow you to easily store the control unit under your bed, both can be used with a smartphone app to track your snoring, and both cost right at $300.
The Nitetronic Clinical Study
 In the “anti-snoring” industry, very few products have been clinically proven to be effective. There are a number of reasons for this, one being the costs associated with conducting a study. Another reason may be because a product simply does not work. Clinical evidence is a strong selling point for any anti-snoring product.
In the “anti-snoring” industry, very few products have been clinically proven to be effective. There are a number of reasons for this, one being the costs associated with conducting a study. Another reason may be because a product simply does not work. Clinical evidence is a strong selling point for any anti-snoring product.
Prior to conducting a study, an empirical test which included 157 people indicated a 67% reduction in snoring.
In December 2014, Nitetronic Europe GmbH conducted a study to determine the effectiveness of their product, Goodnite. The study was conducted by Dr. Uwe Mehrmann from Nitetronics and supervised by Dr. Joachim T. Maurer at the University ENT Clinic at Mannheim sleep lab.
It was a controlled crossover study that examined how changing the position of the head may affect snoring. Participants stayed overnight in a sleep lab for two consecutive nights during this study. The first night they slept with a pillow that was inactive (did not move) while the second night they slept with an active Goodnite pillow. Participants were both men and women over the age of 18 with a BMI of less than 30.
A polysomnography (PSG) study was conducted and the patients were asked about their experiences.
The results were very convincing. There was a significant decrease in the snoring index when the pillow was being used. The conclusion – the snoring of every patient was greatly reduced and the sleep and breathing-related parameters were unaffected. In other words, it reduced snoring without compromising sleep.
My Experience Testing Out the Nitetronic GoodNite Smart Pillow
The Nitetronic clinical study was convincing enough that it persuaded me to try out the Goodnite pillow myself and see how it compared to other snoring treatments that I am familiar with such as the snoring mouthpiece.
The Arrival
 The GoodNite Pillow arrived in a large shipping box and was carefully packed inside of a retail box. Once the box was opened, it revealed a soft pillow with a braided line exiting from the center, which contained what I assumed to be the tubing that inflates the air chambers as well as the sensors which pick up the sound of snoring. This line was connected to the control unit which was packed to the right of the pillow in a separate compartment. The package also contained an instructional manual which was written in several different languages.
The GoodNite Pillow arrived in a large shipping box and was carefully packed inside of a retail box. Once the box was opened, it revealed a soft pillow with a braided line exiting from the center, which contained what I assumed to be the tubing that inflates the air chambers as well as the sensors which pick up the sound of snoring. This line was connected to the control unit which was packed to the right of the pillow in a separate compartment. The package also contained an instructional manual which was written in several different languages.
Before reading over the instructions, I had to know what was inside of the pillow. When I grabbed a hold of it, I noticed that it was very soft and cozy. A zipper on both the left and right sides of the pillow allowed me to take a closer look inside. Inside of the pillow were three additional zippers – one at the top, one at the bottom and one in the center. The upper and lower zipper compartments were filled with an extremely soft polyester material. I noticed that the top portion contained more filler than the bottom which makes sense because if they were filled equally, the profile would be very high.
At the center was the inflatable unit which is responsible for moving the head to prevent snoring. I wanted to take a closer look inside but there was a lock holding the two zippers together. Additionally, there was a tag that read “Do not open”. I was able to hold the unit up to the light and see that there were six distinctive chambers which ran across the entire span of the insert. Additionally, there was a thin piece of perforated foam running across the six air chambers. After examining the pillow, I zipped everything back up and moved on to looking at the rest of the unit.
The braided line leading the pillow measured just over 5′ in length which should be plenty to reach under my bed.
Attached to the braided line was the control unit which contained the brains as well as the working parts such as the pump that sent air through the tubing which inflates and deflates the bags. The control unit is rather large in size, measuring approximately 11″ X 6″ X 3.5″. At one end was the On/Off switch. The braided line exited from the other end and a DC power port was located nearby which allows you to plug into the 5v power adapter that is provided.
The top of the unit had a Bluetooth button which I’m assuming is used to connect the nitetronic pillow to a smartphone. The bottom of the control unit had large rubber feet which help to prevent the unit from easily sliding.
After examining all components, my overall impression was that the Goodnite pillow was well engineered and made from quality materials.
I was anxious to get started but first needed to read over the instructional manual.
The user manual was thicker than expected, but after opening it I quickly realized why. Since the Nitetronic is sold worldwide, the instructions are printed in several different languages. In fact, of the 54 total pages, only 5 pages were printed in English. Surprisingly, the quick start instructions only required 3 steps:
- Connect the power supply to the main unit.
- Place the pillow on your bed.
- Turn on.
I was expecting the setup to take several minutes and require many adjustments, but no – it was ready to use in literally two minutes.
The manual suggested allowing 5-10 nights to become accustomed to sleeping with their pillow. Since I planned on using the Goodnite pillow for several nights, this should allow plenty of time to become adjusted.
Getting Started
As mentioned, the initial setup was quite simple. In order to test it, I recreated the sound of snoring. After three or so loud snores, I suddenly felt my head slowly lifting up on one side. As I continued to make the snoring sound, the air bladder continued to inflate very slowly and my head starts to shift to the side. A few minutes later I tested it again and the opposite side of the pillow inflated, shifting my head the opposite direction. It was interesting to see how the unit responded to the replicated sound of snoring. I also found it interesting how quiet the control unit pump was. The sound was virtually undetectable. Pump noise was a concern of mine at first but this was no longer the case.
Method
When testing the effectiveness of all anti-snoring device, I always spend at least 14 nights putting it to the test to ensure that I’m able to:
- Determine if it works and
- Discover any issues that may exist.
To start off I decided to test the Nitetronic pillow by itself for the first 3 night, without pairing it with my smartphone. The idea is that this information would be helpful to those who do not own a smartphone or are not interested in using the app.
As for measuring the effectiveness of the Nitetronic without the app, I’ll have to rely on my wife who sleeps next to me each night. She typically stays up much later than I do, so she will be able to tell me whether or not it’s working within the first ten minutes of me falling asleep.
For the remaining 11 nights, I will measure the effectiveness using the Nitelink2 which is a free app that is available for both Android and Mac users.
The Results

Nights 1-3
Before going to bed, I had turned the control unit on and laid my head at the center of the pillow. The pillow was rather soft and comfortable. I would even go as far as saying that the pillow was more comfortable than the one that I was currently using.
While laying waiting to fall asleep, I didn’t notice the pillow inadvertently activating which was, of course, a good sign.
It wasn’t long before I was sound asleep with my wife monitoring my snoring closely. Within seconds of the start of my snoring, the pillow activated and slowly raised and rotated my head until the sound of snoring slowly diminished. Thereafter, if I started snoring again, the pillow would begin making adjustments in order to silence the sound of snoring.
The first three nights went well. My snoring was kept at bay and my wife had approved.
Nights 4-6
Over the next 3 nights, I decided to test the capabilities of the Nitelink2 app that had I downloaded to my smartphone.
The instructions indicate that you should spend the first three or so nights recording your snoring with the pillow deactivated, meaning that it will inflate or deflate. The enables you to establish a baseline in which you can compare the nights in which the pillow is activated. That being said, I went into the settings and deactivated the pillow. In addition to deactivating the pillow, I had also set a schedule which allowed it to record from my bedtime of around 11 pm until 7 am the following morning.
After the first night, I went back and reviewed all of the data that was collected throughout the night. It was very interesting to see the percentage of the night in which I snored as well as my sleep efficiency and snoring index. The app even kept track of my snoring intensity, snoring count, and the longest snoring. I was somewhat surprised to hear that I was spent so much of my night snoring.
The following two nights in “inactive” mode showed similar data. The data confirmed what I already knew which is that I snore, and I snore a lot.
Nights 7-14
Now that I had established a 3-day baseline, I was curious to see the quantitative results with the pillow activated and compare this information to what to the prior three days. Before going to bed, I went into the settings and reactivated the pillow.
Over the next eight nights, there was a stark difference percentage-wise between the first three nights when it was deactivated and the following eight nights activated. This information was enough to confirm the effectiveness of the Nitetronic Pillow.
Concluding Thoughts and Recommendations
After two weeks of testing GoodNite anti-snoring smart pillow, the results have proven that it’s, in fact, an effective product. During my trial, the Goodnite pillow had proven itself night after night using both observations as well as recorded data. Overall, I had a great experience which exceeded my expectations. Nitetronics lived up to all of their claims, which is a breath of fresh air in an industry where so many anti-snoring products fail to meet expectations.
As for the $300 price tag, the look, and feel of what you receive justify the cost. It’s a quality product that’s German engineered and well crafted. If the cost of the Goodnite pillow vs performance is a concern, you can rest assured with a risk-free 30-night trial. This will give you more than enough time to decide if this product is a good fit for you.
One of the most attractive features of the Goodnite pillow is the fact that it’s the only clinically proven anti-snore pillow with smart technology. Being clinically proven is a strong selling point that gives this product credibility.
 Due to the fact that it’s clinically proven, high quality comes with a risk-free trial and is easy to use, I have decided to give it my highest recommendation when it comes to smart pillow technology.
Due to the fact that it’s clinically proven, high quality comes with a risk-free trial and is easy to use, I have decided to give it my highest recommendation when it comes to smart pillow technology.
Pros:
- Easy setup / easy use
- Clinically proven to work
- Personally tested and proven effective
- Non-invasive snoring solution
- German engineered and well crafted
- Air pump is virtually silent
- Offered with a 30-night risk-free trial
- Allows you to establish a baseline to compare snoring before & after
- Can be used independently or with smartphone app
- Inflation systems and sensors are integrated into a comfortable pillow
Cons:
- $50 restocking fee if returned
- Not a suitable replacement for CPAP
Share This Post:


 One product that is often mentioned is the anti-snoring pillow. In recent years, numerous snoring pillows have entered the market, capturing the attention of millions of snorers from all around.
One product that is often mentioned is the anti-snoring pillow. In recent years, numerous snoring pillows have entered the market, capturing the attention of millions of snorers from all around. Standard snoring pillows come in a variety of different shapes, sizes, and materials. They are designed to help facilitate sleeping on one’s side. How does side sleeping help to prevent snoring?
Standard snoring pillows come in a variety of different shapes, sizes, and materials. They are designed to help facilitate sleeping on one’s side. How does side sleeping help to prevent snoring? In recent years, we have seen nearly every product transformed into a “smart” version which promises to deliver better results in comparison to its predecessor by making adjustments, collecting information, and storing it on a smartphone app. The snoring pillow is no exception.
In recent years, we have seen nearly every product transformed into a “smart” version which promises to deliver better results in comparison to its predecessor by making adjustments, collecting information, and storing it on a smartphone app. The snoring pillow is no exception. The idea behind the anti-snoring pillow seems plausible but the question is, do anti-snoring pillows really work?
The idea behind the anti-snoring pillow seems plausible but the question is, do anti-snoring pillows really work?

 While not exactly it’s intended use, some mouthpiece users have found that a chinstrap can serve as a useful tool when it comes to holding a mouthpiece in.
While not exactly it’s intended use, some mouthpiece users have found that a chinstrap can serve as a useful tool when it comes to holding a mouthpiece in. You might be wondering if it’s possible to completely forgo the mouthpiece all together and just use a chinstrap. Is this even a possibility?
You might be wondering if it’s possible to completely forgo the mouthpiece all together and just use a chinstrap. Is this even a possibility?





 The GoodNite is a queen size pillow, measuring 24″ X 14.5″ X 3″. The pillow can be fitted with a standard pillowcase which can be exchanged to keep it clean and fresh.
The GoodNite is a queen size pillow, measuring 24″ X 14.5″ X 3″. The pillow can be fitted with a standard pillowcase which can be exchanged to keep it clean and fresh. The technology behind the Goodnite pillow is indeed fascinating but this leaves one very important question – How does slowly moving the head to the side while asleep prevent snoring?
The technology behind the Goodnite pillow is indeed fascinating but this leaves one very important question – How does slowly moving the head to the side while asleep prevent snoring? How much do you expect to pay for such a product? It seems as if a lot of effort and capital have been invested in bringing this device to market, so I wouldn’t expect it to be inexpensive. The retail price for the GoodNite pillow is currently set at $299. Nitetronic does offer free shipping which is, of course, nice considering that it’s a fairly large investment.
How much do you expect to pay for such a product? It seems as if a lot of effort and capital have been invested in bringing this device to market, so I wouldn’t expect it to be inexpensive. The retail price for the GoodNite pillow is currently set at $299. Nitetronic does offer free shipping which is, of course, nice considering that it’s a fairly large investment.
 In the “anti-snoring” industry, very few products have been clinically proven to be effective. There are a number of reasons for this, one being the costs associated with conducting a study. Another reason may be because a product simply does not work. Clinical evidence is a strong selling point for any anti-snoring product.
In the “anti-snoring” industry, very few products have been clinically proven to be effective. There are a number of reasons for this, one being the costs associated with conducting a study. Another reason may be because a product simply does not work. Clinical evidence is a strong selling point for any anti-snoring product. The GoodNite Pillow arrived in a large shipping box and was carefully packed inside of a retail box. Once the box was opened, it revealed a soft pillow with a braided line exiting from the center, which contained what I assumed to be the tubing that inflates the air chambers as well as the sensors which pick up the sound of snoring. This line was connected to the control unit which was packed to the right of the pillow in a separate compartment. The package also contained an instructional manual which was written in several different languages.
The GoodNite Pillow arrived in a large shipping box and was carefully packed inside of a retail box. Once the box was opened, it revealed a soft pillow with a braided line exiting from the center, which contained what I assumed to be the tubing that inflates the air chambers as well as the sensors which pick up the sound of snoring. This line was connected to the control unit which was packed to the right of the pillow in a separate compartment. The package also contained an instructional manual which was written in several different languages.
 Due to the fact that it’s clinically proven, high quality comes with a risk-free trial and is easy to use, I have decided to give it my highest recommendation when it comes to smart pillow technology.
Due to the fact that it’s clinically proven, high quality comes with a risk-free trial and is easy to use, I have decided to give it my highest recommendation when it comes to smart pillow technology.



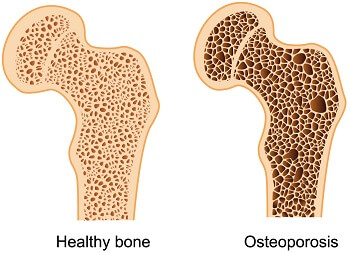 Osteoporosis is a common bone disease that occurs when bone density is reduced, causing bones to become weak and brittle. It’s most common in people who are older than 50 and the diagnosis often comes as a surprise after one breaks a bone. It’s estimated that over fifty million Americans are affected by this condition. The disease is more common in women – affecting nearly 50% while only 25% of men are affected.
Osteoporosis is a common bone disease that occurs when bone density is reduced, causing bones to become weak and brittle. It’s most common in people who are older than 50 and the diagnosis often comes as a surprise after one breaks a bone. It’s estimated that over fifty million Americans are affected by this condition. The disease is more common in women – affecting nearly 50% while only 25% of men are affected. Yet another common medical condition is being linked with sleep apnea – Arthritis.
Yet another common medical condition is being linked with sleep apnea – Arthritis.
 Routinely waking up each morning with an unexpected headache is a concern that should be appropriately addressed as it may be an indicator of an underlying condition.
Routinely waking up each morning with an unexpected headache is a concern that should be appropriately addressed as it may be an indicator of an underlying condition.
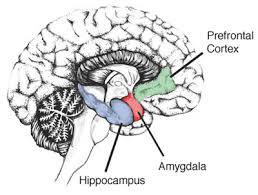
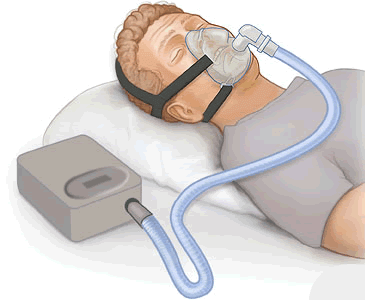 Long considered the “gold standard” of OSA treatment, the Continues Positive Airway Pressure (CPAP) therapy is one of the most prescribed treatment methods for OSA. With CPAP therapy, a continuous stream of air is delivered to the face from a CPAP machine. This stream of air effectively “blows open” the airway which treats the obstruction and allows normal breathing to occur.
Long considered the “gold standard” of OSA treatment, the Continues Positive Airway Pressure (CPAP) therapy is one of the most prescribed treatment methods for OSA. With CPAP therapy, a continuous stream of air is delivered to the face from a CPAP machine. This stream of air effectively “blows open” the airway which treats the obstruction and allows normal breathing to occur. As the name implies, Oral Appliance Therapy involves therapy that uses an oral appliance or mouthpiece. A physician will create a custom fitted mouthpiece that works by holding the mandible forward. In doing so it helps by relieving pressure from the airway caused by the jaw falling backward at night.
As the name implies, Oral Appliance Therapy involves therapy that uses an oral appliance or mouthpiece. A physician will create a custom fitted mouthpiece that works by holding the mandible forward. In doing so it helps by relieving pressure from the airway caused by the jaw falling backward at night.



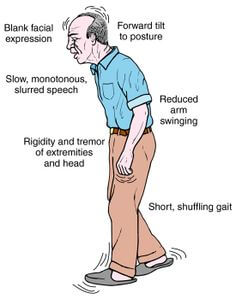
 ith Parkinson’s are loud snorers as well, a symptom of sleep apnea.
ith Parkinson’s are loud snorers as well, a symptom of sleep apnea. 
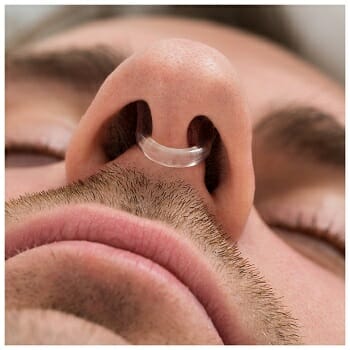 Nasal cones are typically made from a soft plastic or silicone material and are made in a number of different shapes. Some, such as Mute or WoodyKnows is a clip style that fit inside of the nose and is designed with rings that expand the nostril out and open. The advantage of the clip style is that it takes up very little room in the nostril which allows for a greater volume of air to flow unobstructed.
Nasal cones are typically made from a soft plastic or silicone material and are made in a number of different shapes. Some, such as Mute or WoodyKnows is a clip style that fit inside of the nose and is designed with rings that expand the nostril out and open. The advantage of the clip style is that it takes up very little room in the nostril which allows for a greater volume of air to flow unobstructed.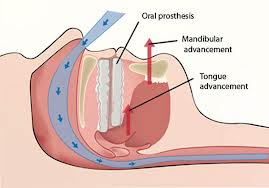 Another popular snoring solution is often referred to as a snoring mouth guard or mouthpiece. Like Nasal cones, mouth guards are also sold by a number of manufacturers such as SleepTight, zQuiet, Good Morning Snore Solution, Zyppah, SnoreRx, PureSleep, and many others. Unlike Nasal cones, mouth guards focus more on opening the airway rather than the nasal passages.
Another popular snoring solution is often referred to as a snoring mouth guard or mouthpiece. Like Nasal cones, mouth guards are also sold by a number of manufacturers such as SleepTight, zQuiet, Good Morning Snore Solution, Zyppah, SnoreRx, PureSleep, and many others. Unlike Nasal cones, mouth guards focus more on opening the airway rather than the nasal passages. Now that we have an understanding of what Nasal cones and mouth guards are and how they work, let’s get down to the million-dollar question which is ‘which product works better to stop snoring?’, the Nasal cone or mouth guard?
Now that we have an understanding of what Nasal cones and mouth guards are and how they work, let’s get down to the million-dollar question which is ‘which product works better to stop snoring?’, the Nasal cone or mouth guard?